Navigating the world of contraceptives can be complex, especially when you’re a nursing mother. Plan B, also known as the “morning-after pill,” is a popular emergency contraceptive that many women consider using after unprotected intercourse or contraceptive failure. However, if you’re breastfeeding, you might be concerned about the potential effects this medication could have on you and your baby. This article aims to demystify Plan B and explore its possible risks and side effects during breastfeeding.
What is Plan B?
Plan B is an over-the-counter emergency contraceptive designed to prevent pregnancy after unprotected sex. Its active ingredient is levonorgestrel, a synthetic hormone that helps prevent ovulation. For Plan B to be most effective, it should be taken as soon as possible after unprotected intercourse, ideally within 72 hours.
The Active Ingredient: Levonorgestrel
Levonorgestrel is a synthetic progestogen that mimics naturally occurring progesterone in the body. This hormone plays a critical role in regulating the menstrual cycle and maintaining pregnancy. By introducing levonorgestrel through Plan B, the body is tricked into delaying ovulation, thereby reducing the chance of conception.
Timing and Effectiveness
The timing of taking Plan B is crucial for its effectiveness. Studies show that taking the pill within 24 hours significantly increases its efficacy compared to later use within the 72-hour window. However, it is important to note that Plan B is not 100% effective and its efficacy decreases the longer you wait after unprotected intercourse.
Distinction from Other Emergency Contraceptives
While Plan B is one of the most well-known emergency contraceptives, it’s important to distinguish it from other options like Ella (ulipristal acetate) or a copper IUD. Each option works differently and may have varying degrees of effectiveness and side effects, especially for breastfeeding mothers.
How Does Plan B Work?
Plan B primarily works by delaying ovulation, thus preventing the release of an egg. Without an egg to fertilize, pregnancy cannot occur. It may also prevent fertilization of an egg if ovulation has already occurred or stop a fertilized egg from implanting in the uterus. It is crucial to understand that Plan B is not an abortion pill and will not affect an existing pregnancy.
Mechanism of Action
The primary mechanism of Plan B is to delay ovulation, which is the release of an egg from the ovary. By delaying this process, Plan B reduces the likelihood of an egg being present for fertilization during intercourse. This is a crucial step in preventing pregnancy.
Secondary Mechanisms
Besides delaying ovulation, Plan B may alter the movement of sperm and egg in the fallopian tubes, thereby reducing the chance of fertilization. Furthermore, it may change the lining of the uterus, making it less receptive to a fertilized egg. These secondary mechanisms add layers of effectiveness to prevent pregnancy.
Clarifying Misconceptions
There are common misconceptions that Plan B can terminate an existing pregnancy. It’s essential to clarify that Plan B does not disrupt an implanted pregnancy; its function is solely preventative. This distinction is critical for understanding its role and limitations as an emergency contraceptive.
Plan B and Breastfeeding: What You Need to Know

by Liana S (https://unsplash.com/@cherstve_pechivo)
For breastfeeding mothers, the primary concern is whether the medication will pass into breast milk and affect the nursing infant. Here is what current research indicates:
Safety of Plan B During Breastfeeding
The active ingredient in Plan B, levonorgestrel, does pass into breast milk in small amounts. However, studies have shown that these amounts are not likely to be harmful to a nursing infant. The World Health Organization and the American Academy of Pediatrics consider levonorgestrel-based emergency contraception to be compatible with breastfeeding.
Research Findings on Safety
Research has demonstrated that the concentration of levonorgestrel in breast milk is minimal and unlikely to cause harm. Studies involving breastfeeding mothers who have taken Plan B show no significant adverse effects on infants. This consensus reassures many nursing mothers concerned about potential drug exposure through breast milk.
Medical Guidelines and Recommendations
Medical bodies such as the WHO and the American Academy of Pediatrics endorse the use of Plan B during breastfeeding. Their guidelines highlight that the benefits of preventing unintended pregnancy outweigh the minimal risk posed by levonorgestrel in breast milk. These endorsements provide a reliable basis for decision-making among nursing mothers.
Addressing Common Concerns
Despite the general safety, some mothers remain apprehensive about using Plan B while breastfeeding. It’s vital to address these concerns by consulting healthcare professionals who can provide personalized advice based on individual health profiles. Open communication with your healthcare provider can alleviate concerns and ensure informed decisions.
Potential Side Effects for Nursing Mothers
While Plan B is generally considered safe, nursing mothers may experience some side effects. These can include:
- Nausea and Vomiting: Some women may feel nauseous after taking Plan B. If vomiting occurs within two hours of taking the pill, you may need to take another dose.
- Fatigue: Feeling tired or experiencing a lack of energy is a common side effect.
- Headache and Dizziness: Some mothers report mild headaches or dizziness.
- Breast Tenderness: You may experience some tenderness in your breasts, although this is usually temporary.
- Menstrual Changes: Plan B can cause your next period to be earlier, later, or heavier than usual.
Managing Nausea and Vomiting
Nausea and vomiting are among the most reported side effects after taking Plan B. To minimize discomfort, consider taking the pill with food or opting for an anti-nausea medication. If vomiting occurs soon after ingestion, a healthcare provider may recommend retaking the dose to ensure effectiveness.
Coping with Fatigue and Headaches
Fatigue and headaches, although generally mild, can disrupt daily routines, especially for new mothers. Staying hydrated and ensuring adequate rest can help alleviate these symptoms. If headaches persist, over-the-counter pain relief may be considered, but it’s advisable to consult a healthcare professional before taking additional medication.
Understanding Menstrual Changes
Plan B can disrupt the regularity of your menstrual cycle, leading to changes in timing and flow. These alterations are typically temporary and should normalize by the next cycle. Tracking your periods post-Plan B can help you anticipate changes and manage expectations.
Effects on Milk Supply
There is limited evidence to suggest that Plan B significantly affects milk production. However, any hormonal changes could potentially impact your milk supply. If you notice a decrease in milk production, it’s advisable to consult a healthcare professional.
Hormonal Impact on Lactation
Hormonal contraceptives can sometimes influence lactation, though Plan B’s impact is generally minimal due to its short-term usage. Any noticeable change in milk supply is often transient and resolves without intervention. Being aware of this potential side effect helps in monitoring and addressing lactation concerns promptly.
Seeking Professional Guidance
Consulting a lactation specialist or healthcare provider can provide insights into any perceived changes in milk supply. They can offer strategies to maintain production, such as increased breastfeeding frequency or pumping sessions. Personalized advice ensures that both mother and baby continue to thrive.
Balancing Contraception and Nursing Needs
Balancing the need for effective contraception with the desire to maintain a healthy milk supply can be challenging. Exploring all contraceptive options, including non-hormonal methods, may help nursing mothers find a solution that aligns with their lifestyle and breastfeeding goals.
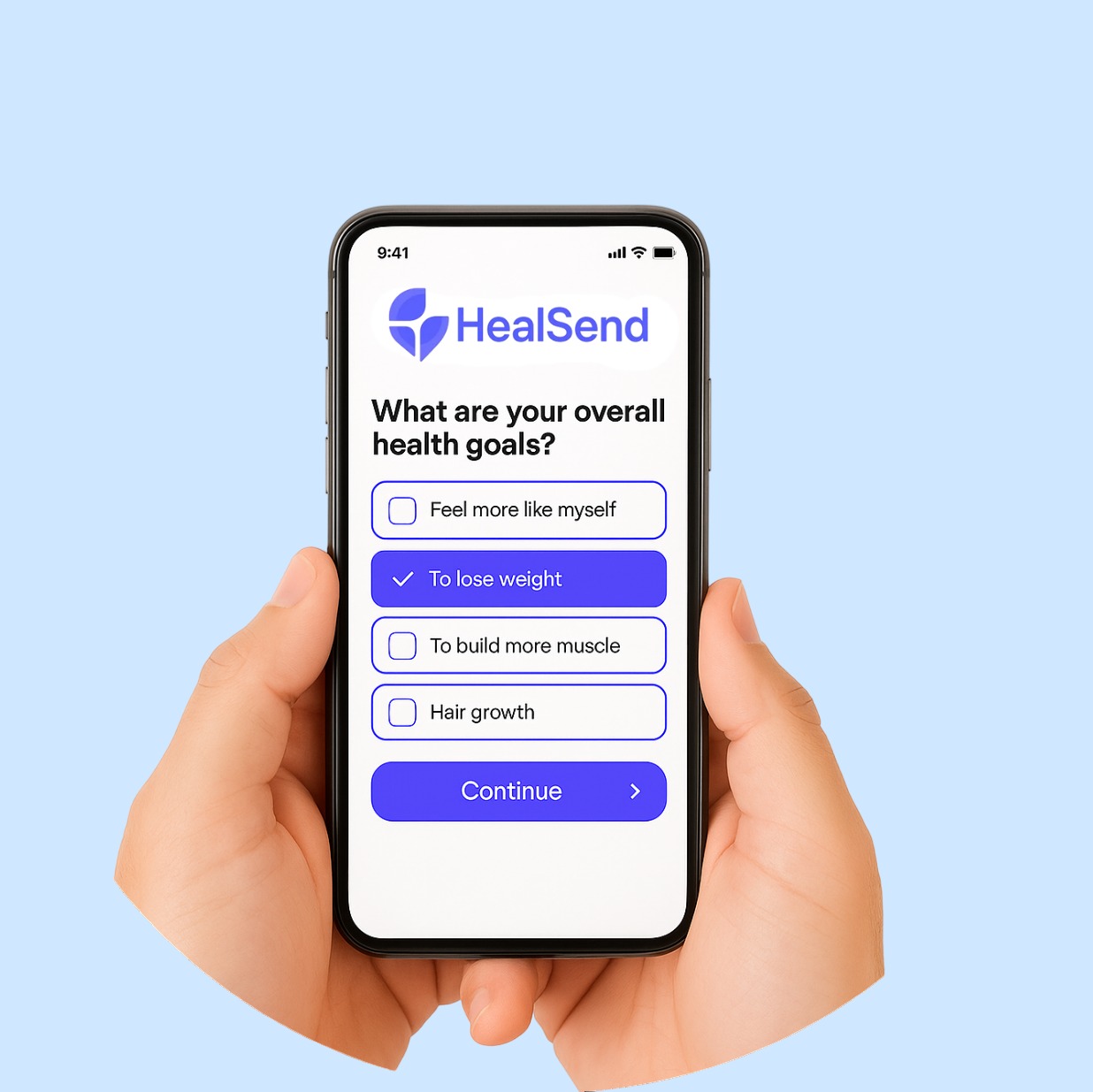
Comparing Plan B to Other Contraceptive Options

by Reproductive Health Supplies Coalition (https://unsplash.com/@rhsupplies)
While Plan B is a convenient option in emergency situations, it is not intended for regular contraceptive use. Here’s how it compares to other methods:
Regular Birth Control Pills
Regular birth control pills contain a combination of hormones and are designed for continuous use. Unlike Plan B, which is a single-dose emergency option, daily birth control pills are taken consistently to prevent pregnancy.
Differences in Hormonal Composition
Regular birth control pills typically contain a combination of estrogen and progestin, whereas Plan B contains only levonorgestrel. This difference in hormonal composition affects how each method regulates the menstrual cycle and prevents pregnancy, with regular pills offering more consistent hormonal control.
Usage and Consistency
The effectiveness of regular birth control pills relies heavily on daily adherence. Missing doses can compromise their effectiveness, unlike Plan B, which is a one-time emergency measure. This distinction underscores the importance of routine for those choosing regular contraceptives.
Potential Impact on Breastfeeding
While regular birth control pills are effective, those containing estrogen may affect milk supply more than progestin-only options like Plan B. Nursing mothers often prefer progestin-only pills or mini-pills to minimize any impact on lactation while ensuring effective contraception.
Intrauterine Devices (IUDs)
IUDs are long-term contraceptive devices inserted into the uterus. They are highly effective and can be used for several years. Some IUDs release hormones similar to those in Plan B, while others are non-hormonal and use copper to prevent pregnancy.
Hormonal vs. Non-Hormonal IUDs
Hormonal IUDs, like Mirena, release levonorgestrel, similar to Plan B, but at a lower, steady rate. Non-hormonal IUDs, such as ParaGard, use copper to create an inhospitable environment for sperm. Both types offer distinct advantages and considerations for breastfeeding mothers.
Duration and Maintenance
IUDs provide long-term contraception, lasting between 3 to 10 years depending on the type. This “set and forget” method is appealing for mothers seeking reliable, low-maintenance contraception. However, insertion requires a healthcare provider, and there may be an adjustment period for the body.
Considerations for Nursing Mothers
For breastfeeding mothers, non-hormonal IUDs may be preferable to avoid potential impacts on milk supply. Hormonal IUDs, although containing levonorgestrel, are generally considered safe and may offer additional benefits like reduced menstrual bleeding.
Condoms and Barrier Methods
Condoms and other barrier methods physically prevent sperm from reaching the egg. These methods do not contain hormones and do not affect breastfeeding or milk supply.
Variety and Accessibility
Barrier methods include male and female condoms, diaphragms, and cervical caps. These options are widely accessible and do not require a prescription, making them a convenient choice for many. Their non-hormonal nature makes them particularly suitable for breastfeeding mothers concerned about milk supply.
Effectiveness and Usage
The effectiveness of barrier methods largely depends on correct and consistent use. Unlike hormonal options, they provide immediate protection without affecting the body’s hormonal balance. However, they do not offer the same reliability as long-term methods like IUDs or pills.
Integration with Other Methods
Barrier methods can be used in conjunction with other contraceptives for added protection. For instance, combining condoms with hormonal methods can reduce the risk of both pregnancy and sexually transmitted infections, providing comprehensive protection for nursing mothers.
When to Consult a Healthcare Professional
While Plan B is generally safe, it’s always wise to consult with a healthcare provider if you have concerns, especially when breastfeeding. They can offer personalized advice and discuss alternative contraceptive options that best suit your lifestyle and health needs.
Situations Requiring Medical Advice
- Severe Side Effects: If you experience severe side effects such as intense abdominal pain or heavy bleeding, seek medical attention.
- Repeated Use: If you find yourself needing Plan B frequently, discuss long-term contraceptive options with your doctor.
- Concerns About Milk Supply: If you notice a significant change in your milk production or your baby’s feeding pattern, a lactation consultant or healthcare provider can offer guidance.
Addressing Severe Side Effects
Experiencing severe side effects after taking Plan B warrants immediate medical attention. Symptoms like intense abdominal pain or heavy bleeding could indicate underlying issues that need to be addressed promptly. A healthcare provider can assess the situation and provide necessary interventions.
Evaluating Frequent Usage
Repeated reliance on Plan B suggests a need for a more consistent contraceptive plan. Frequent use may not be sustainable or ideal for long-term reproductive health. Consulting a healthcare provider can help explore alternative methods that align better with your lifestyle and breastfeeding needs.
Monitoring Milk Supply and Infant Health
Any noticeable changes in milk supply or your infant’s feeding pattern should prompt a consultation with a healthcare professional. They can assess whether these changes are linked to Plan B or other factors, providing reassurance and support for continued breastfeeding success.
Benefits of Professional Guidance
Consulting with healthcare professionals offers numerous benefits, including tailored advice and reassurance. They can help navigate the complex landscape of contraceptive options, addressing both your reproductive health and breastfeeding goals. Open dialogue ensures informed and confident decision-making.
Final Thoughts
Understanding how Plan B interacts with breastfeeding is crucial for making informed decisions about emergency contraception. While studies suggest that it is generally safe for nursing mothers, it’s important to weigh the benefits and potential risks. Always consider consulting healthcare professionals when uncertain about medication use during breastfeeding.
Empowerment Through Knowledge
Informed choices empower you to protect both your reproductive health and your child’s well-being. By staying informed about the latest research and recommendations, you can confidently navigate contraceptive options while breastfeeding. Knowledge equips you to make decisions that align with your health and family goals.
Navigating Future Choices
As new contraceptive methods and research emerge, staying updated ensures that you continue to make the best choices for your evolving needs. Engaging with healthcare providers and accessing reputable resources can support ongoing education and adaptability in your contraceptive journey.
Encouragement for Open Communication
Open communication with healthcare providers fosters a supportive environment for discussing contraceptive options and breastfeeding concerns. By expressing your needs and preferences, you can work collaboratively to find solutions that enhance your health and well-being.